What to know about the Listeria outbreaks in the US and Canada
Cases of listeriosis, spread by the bacteria known as “listeria monocytogenes”, have led to four deaths so far in the US and Canada.
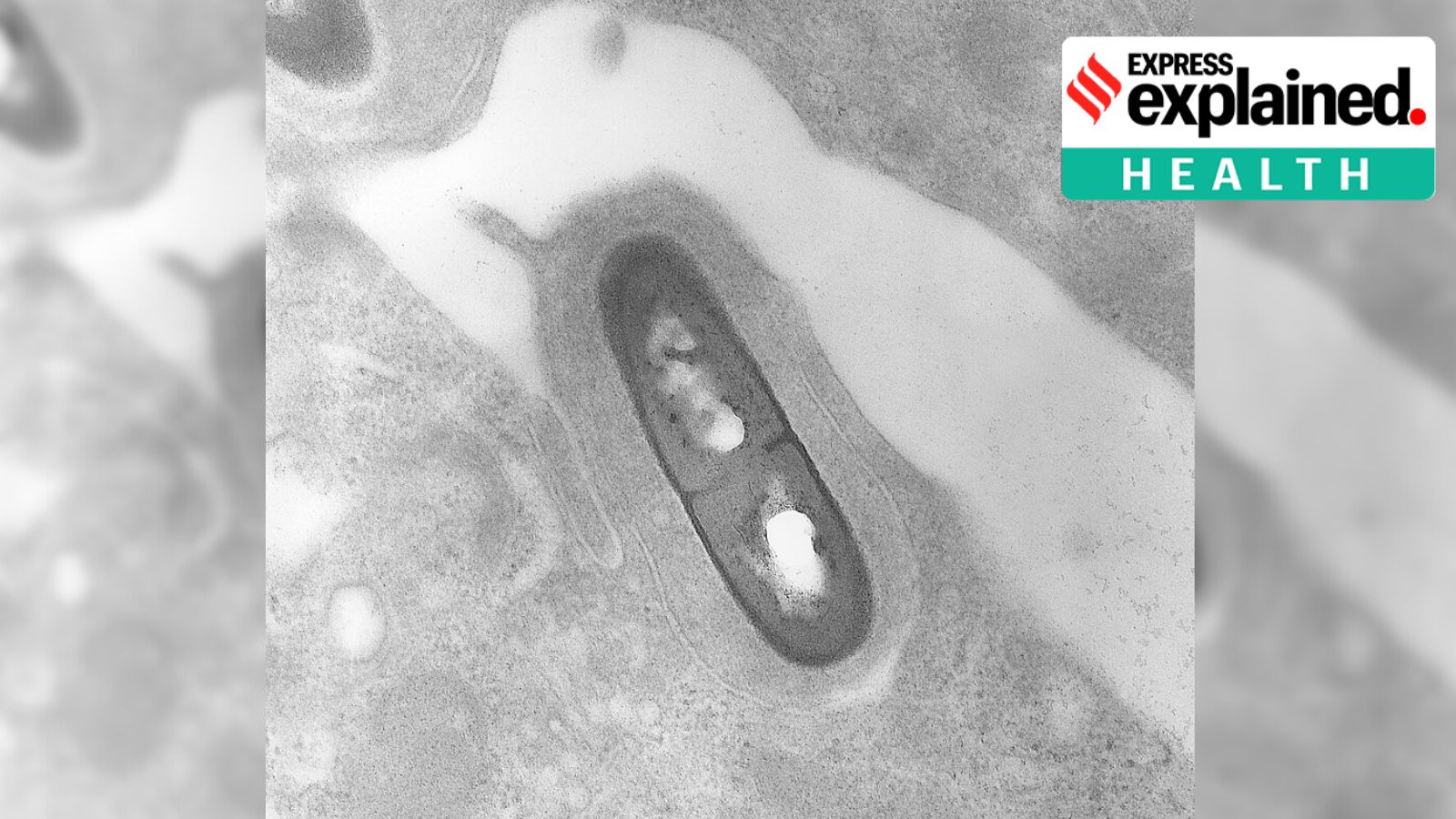 Electron micrograph of Listeria monocytogenes bacterium in tissue. (Photo - Wikimedia Commons)
Electron micrograph of Listeria monocytogenes bacterium in tissue. (Photo - Wikimedia Commons)Two separate outbreaks of listeria, a bacteria which can contaminate food, have been reported in the United States and Canada in recent weeks. The US government’s Centers for Disease Control and Prevention (CDC) on July 19 reported an outbreak across 12 states, attributing it to the consumption of undercooked meats sliced at deli counters. Two deaths have been reported, while 28 people have been hospitalised.
The Canadian government’s public health notice on July 17 said 12 cases had been reported and two of them resulted in deaths. Here is what to know.
What is listeria and listeriosis?
Listeria or Listeria monocytogenes is a type of bacteria found in soil, vegetation, water, sewage and even the faeces of animals and humans. Listeria-contaminated food can lead to an infection called listeriosis.
What are the symptoms of listeriosis?
Most people who ingest listeria-infected food do not fall sick or develop symptoms. The bacteria can be present in the infected person’s system for up to two months until the symptoms present themselves, making it difficult to establish the connection between what was consumed and the infection.
Symptoms include vomiting, nausea, cramps, severe headache, constipation and fever.
Who is vulnerable to listeriosis?
People with compromised immune systems, pregnant persons and their offspring and the elderly (aged 65 and above) are vulnerable. The US outbreak has a median age of 75. Listeria can result in hospitalisation and even death for the immunocompromised and the elderly.
According to the CDC, pregnant women are 10 times more likely to develop a listeria infection and risk pregnancy loss, premature birth or even life-threatening infection in the newborn.
Some foods are more likely to have listeria than others, including milk, raw sprouts, deli meats and hot dogs, soft cheeses and smoked seafood.
What is the treatment for listeriosis?
Treatment depends on the extent of the infection. In many cases, intestinal listeriosis manifests within a day or two of consuming the contaminated food item and may lead to diarrhoea and vomiting. The treatment is similar to one for a routine stomach infection and could require antibiotics.
If the infection spreads beyond the intestines, it leads to invasive listeriosis. Severe symptoms present themselves two weeks after the food has been consumed.
What do we know about the listeria outbreaks?
The CDC says, “When two or more people get the same illness from the same contaminated food or drink, the event is called a foodborne disease outbreak”.
The true numbers of those infected may be higher than reported as the symptoms are not immediately visible. Some people may recover without medical care.
Of the 18 infected people the CDC interviewed, 16 had consumed meat sliced at a deli. The US Department of Agriculture’s Food Safety and Inspection Service (USDA-FSIS) is working to identify the deli meat suppliers responsible. No product recalls have been announced so far and a CDC investigation is underway.
In neighbouring Canada, a separate listeria outbreak is reportedly connected to the contamination of plant-based refrigerated beverages, including the Danone’s Silk brand and the Great Value brand of drinking milk substitutes (almonds, oats, cashews and coconuts).
About 15 items under the Silk brand were recalled on July 8 by the Canada Food Inspection Agency (CFIA), the regulatory body responsible for monitoring the quality of food items.
There are concerns it may be similar to a 2008 outbreak when contaminated cold cuts from Maple Leaf Foods, one of Canada’s largest meatpackers, left 22 dead and 57 ill. The extent of the current outbreak has not been detailed yet.
On its website, Silk said on July 17 that the contaminated drinks were made by a third-party facility, with a preventative recall being issued on all Silk refrigerated beverage products as the investigation continues.
Has any advisory been issued?
The CDC has advised the public, especially high-risk groups, to avoid unheated deli meats, cheeses and salads and opt for packaged items instead. Deli equipment, surfaces and food can be easily contaminated, while refrigeration of deli items does not kill the bacteria. All deli meats are recommended to be heated to an internal temperature of 165 degrees F before consumption to kill Listeria, if present.
Refrigerators, containers and surfaces that have come into contact with deli meats are advised to be thoroughly sanitised. Finally, all patients displaying symptoms, especially those in the high-risk groups, are advised to seek medical attention immediately.
- 01
- 02
- 03
- 04
- 05