Her experience is far from unique. Across India, millions live with the condition without realising it until it’s too late. According to a 2021 study published in Henry Ford Health Scholarly Commons, “Prevalence of osteoporosis ranging from 8 to 62 per cent in Indian women of different age groups has been reported in several studies. In males over 50, prevalence varies between 8.5 and 24.6 per cent.”

The invisible threat
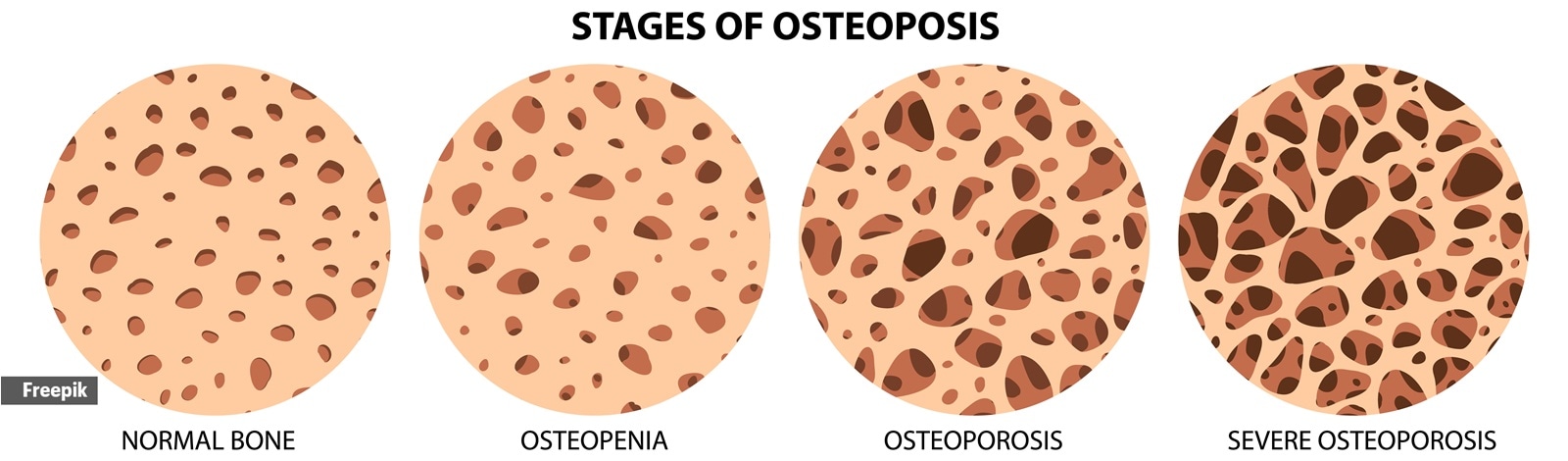
Osteoporosis has earned the label of a “silent epidemic” for good reason. Dr Abhijit Agashe, consultant orthopaedic and joint replacement surgeon at Sahyadri Super Speciality Hospital, Pune, explains: “It’s a ‘silent’ pathology with non-specific symptoms. Patients normalise back pain, height loss, or fatigue. Primary care often prioritises diabetes, blood pressure, and lipids; bone health is usually an afterthought.”
Story continues below this ad
The consequences of this invisibility can be severe. Dr (Prof.) Raju Vaishya, senior consultant orthopaedic and joint replacement surgeon at Indraprastha Apollo Hospitals, New Delhi, notes, “Most patients are asymptomatic until their first fracture, leading to under-recognition.”
Limited infrastructure further compounds the problem. “In smaller cities, DXA scans, which measure bone density, are not easily available, and even where they are, cost is prohibitive,” says Dr Agashe. “Many people take vitamin D and calcium supplements on their own without first checking their actual levels.”
Why Indians are more vulnerable
India’s population faces a unique constellation of risk factors that make osteoporosis more prevalent. Dr Agashe points to several dietary and lifestyle patterns: “Our diets are often low in calcium, and cereals like wheat and rice can reduce calcium absorption. Vitamin D deficiency is widespread due to limited sun exposure, pollution, and cultural clothing practices.”
Dr Vaishya echoes this, adding, “High prevalence of vitamin D deficiency, low dietary calcium intake, and lifestyle habits all contribute.”
Story continues below this ad
Nutritionist Aditi Prabhu, founder of NutroDynamix, notes additional dietary pitfalls: high consumption of polished grains, ultra-processed foods, low protein intake, insufficient calcium-rich foods, and excessive tea, coffee, and salt — all of which compromise bone health.
For women, risks multiply. “Indian women often undergo early menopause and multiple pregnancies, both of which reduce bone strength,” says Dr Agashe. Dr Vaishya adds, “Postmenopausal decline in oestrogen accelerates bone loss. Lifetime calcium deficiency, poor nutrition, and early menopause all contribute significantly.”
 Indian women often undergo early menopause and multiple pregnancies, both of which reduce bone strength (Source: Freepik)
Indian women often undergo early menopause and multiple pregnancies, both of which reduce bone strength (Source: Freepik)
Daily struggles
For those diagnosed, osteoporosis alters everyday life. Praveen explains, “It has definitely slowed me down. I can’t stand for long periods, and even simple tasks require frequent breaks. Eating very cold foods often triggers bone pain. I carry a crepe bandage to ease discomfort in my foot.”
Lakshmi, 64, shares a similar story: “My mobility is reduced by 20–30 per cent, so I rely on others for certain tasks. I have to manage pain while taking calcium supplements twice daily.” Her son, Sudarshan Venkat, adds that while osteoporosis affects her mobility, other conditions like autoimmune disorders and rheumatoid arthritis also play a role.
Story continues below this ad
The mental health impact
The psychological toll of osteoporosis is often overlooked. Praveen admits, “I feel anxiety and frustration, especially when pain limits movement. Missing my daily walk or exercise routine makes me feel low or anxious about gaining weight or becoming more prone to other health issues. There’s always a subtle fear of fractures in the back of my mind.”
Neha Parashar, clinical psychologist at Mindtalk, explains, “Constant awareness of fragility and the possibility of fractures can lead to persistent anxiety, avoidance of activities, and low mood.”
Sakshi Mandhyan, psychologist and founder of Mandhyan Care, calls it the “fear-avoidance cycle”: “People avoid activity out of fear of falling, which reduces strength and balance, ironically increasing fracture risk. Loss of independence also affects identity and self-worth.”
For women, societal expectations add another layer. Parashar notes, “Osteoporosis coincides with postmenopausal changes and societal expectations around strength and independence, which can impact self-image.” Mandhyan adds, “Women often face a double burden: the condition is more prevalent post-menopause and intersects with caregiving expectations.”
Story continues below this ad
Dr Vaishya confirms, “Fractures contribute to depression, anxiety, and social withdrawal due to loss of function.”
The cost of late diagnosis
Discovering osteoporosis only after a fracture can be psychologically devastating. Mandhyan calls it “adjustment stress,” where patients suddenly struggle with a new health reality. Parashar adds, “Transitioning from perceiving oneself as healthy to being labelled fragile triggers intense distress. Misinterpreting early symptoms as ageing delays intervention and increases frustration.”
Physically, consequences can be severe. Dr Agashe warns, “Hip fractures can lead to long hospital stays, reduced mobility, and higher risk of death within a year. Spine fractures can cause back pain, hunching, breathing issues, and repeated falls. After one fracture, the risk of additional fractures rises sharply.”
 Balanced meals with whole grains, seasonal fruits and vegetables, adequate protein, and calcium-rich foods like sesame and ragi are essential. (Source: Freepik)
Balanced meals with whole grains, seasonal fruits and vegetables, adequate protein, and calcium-rich foods like sesame and ragi are essential. (Source: Freepik)
Prevention and management
Despite challenges, actionable steps exist. Praveen says, “Staying active is key, even with pain. I walk gently, rotate joints slowly, take calcium and Vitamin D supplements, and maintain a balanced diet.”
Story continues below this ad
Dr Vaishya recommends weight-bearing exercises, muscle strengthening, and balance training. Dietary advice focuses on adequate calcium, protein, Vitamin D, and reducing salt and caffeine intake.
Nutritionist Prabhu adds, “Balanced meals with whole grains, seasonal fruits and vegetables, adequate protein, and calcium-rich foods like sesame and ragi are essential. Supplements are not a replacement for food and should be taken only under medical guidance.”
Addressing the mental health factor
Parashar advocates integrating psychological support: “Counselling, CBT, and support groups help patients process fears and adapt to lifestyle changes. Collaboration between orthopaedists, physiotherapists, and psychologists ensures holistic care.”
Mandhyan stresses support networks: “Support groups replace isolation with shared strength. Graded activity builds confidence so people can re-engage with movement without overwhelming fear.”
Story continues below this ad
The road ahead
Systemic gaps are clear. Dr Agashe highlights the need for national guidelines, affordable scans, food fortification, and awareness campaigns. Dr Vaishya adds, “Lack of screening programs and low insurance coverage hinder timely diagnosis. Social stigma around fractures prevents open discussion and proactive management.”
Praveen concludes, “I wish there were more awareness about preventive checkups, especially for women. Regular screening can help detect osteoporosis early.”
As India’s population ages, osteoporosis will only become more prevalent. The question is whether it will continue to be discovered through painful fractures — or whether bone health will finally receive the attention it deserves.
DISCLAIMER: This article is based on information from the public domain and/or the experts we spoke to. Always consult your health practitioner before starting any routine.



 Indian women often undergo early menopause and multiple pregnancies, both of which reduce bone strength (Source: Freepik)
Indian women often undergo early menopause and multiple pregnancies, both of which reduce bone strength (Source: Freepik) Balanced meals with whole grains, seasonal fruits and vegetables, adequate protein, and calcium-rich foods like sesame and ragi are essential. (Source: Freepik)
Balanced meals with whole grains, seasonal fruits and vegetables, adequate protein, and calcium-rich foods like sesame and ragi are essential. (Source: Freepik)

























