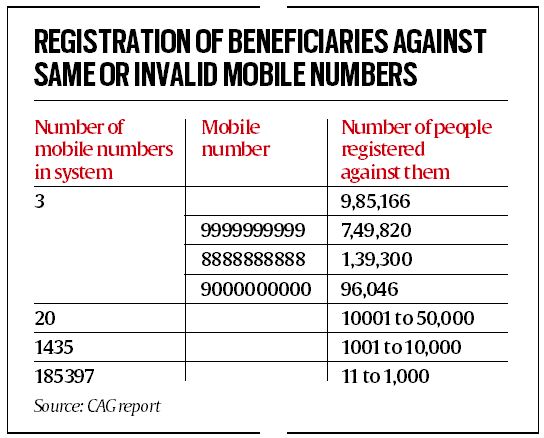
“Data analysis of the BIS database revealed that there were large numbers of beneficiaries registered against the same or invalid mobile number. Overall, 1119 to 7,49,820 beneficiaries were linked with a single mobile number in the BIS database…,” the report states.
Besides 7,49,820 beneficiaries linked with 9999999999, 1,39,300 beneficiaries were linked to the phone number 8888888888; and 96,046 others linked to the number 9000000000.
There were also at least 20 cellphone numbers to which between 10,001 and 50,000 beneficiaries were linked, as per the report.
The report stated that 7.87 crore beneficiary households were registered, constituting 73% of the targeted households of 10.74 crore (November 2022). Later, the government increased the target to 12 crore.
The report noted, “Mobile numbers are significant for searching records related to any beneficiary in the database, who may approach the registration desk without the ID. In case of loss of e-card, identification of the beneficiary may also become difficult. This may result in denial of scheme benefits to eligible beneficiaries as well as denial of pre- and post-admission communication causing inconvenience to them.”

Story continues below this ad
“The NHA [National Health Authority], while agreeing with audit observation, stated (August 2022) that with the deployment of BIS 2.0, this issue shall be resolved,” the CAG reported. “Further, the BIS 2.0 system has been configured so that more than a certain number of families cannot use the same mobile number. This shall arrest the prevalence of entering ‘random numbers’ which constitute the overwhelming cases of mobile number inconsistency.”
According to the report, “Beneficiary Empowerment Guidebook provides that for communication with the beneficiary from admission in hospital to post-discharge feedback, contact number will be used.”
”Guidelines on disabling a BIS e-card provides that the SHA shall send SMS intimation to the contact number provided at the time of card creation informing the beneficiary to check their eligibility. Data analysis of the BIS database revealed that there were large numbers of beneficiaries registered against the same or invalid mobile number,” it states.
The report has also pointed out unrealistic household size for registered beneficiaries under PMJAY. “Data analysis revealed that in 43,197 households, the size of the family was unrealistic, ranging from 11 to 201 members…” the report noted. “Presence of such unrealistic members in a household in the BIS database indicates not only lack of essential validation controls in the beneficiary registration process, but also the possibility that beneficiaries are taking advantage of the lack of a clear definition of family in the guidelines.”
Story continues below this ad
“NHA, while accepting the audit observation, stated (August 2022) that the National Anti-Fraud Unit has sent periodic reminders to the States/UTs highlighting discrepancies in verified data. However, ‘Public Health’ being a State subject, the final decision in this regard vests with the State Governments,” the report stated. “Also, NHA is developing a policy to disable ‘Add Member’ functionality in case of any beneficiary family with more than 15 members.”
According to the report, many pensioners in Chandigarh, Haryana, Himachal Pradesh, Karnataka, Maharashtra and Tamil Nadu were found possessing PMJAY cards and availing treatment under the scheme.
In Tamil Nadu, a comparison of the state government’s pensioner database with the scheme database showed that “1,07,040 pensioners were included as beneficiaries”, the report noted. “The premium paid by SHA to insurance company for these pensioners worked out to Rs 22.44 crore.”
“Audit observed that delayed action in weeding out the ineligible beneficiaries resulted in ineligible persons availing benefits of the Scheme and excess payment of premium to the insurance companies,” the report stated.
Story continues below this ad
“NHA, while accepting the audit observation, replied (August 2022) that it is developing an SOP for adherence by the States to ensure that any SECC 2011 beneficiary family found ineligible as per AB-PMJAY criteria can be removed from the list of eligible individuals/families,” it added.