📣 For more lifestyle news, click here to join our WhatsApp Channel and also follow us on Instagram
What it’s like to have pulmonary tuberculosis in modern-day India: ‘I remember calling my mother at 3 AM…’
Once known as a disease of the past, tuberculosis continues to haunt modern India — with delayed diagnoses, stigma, and stories of resilience that reveal how little has changed beneath the surface.
 Pulmonary TB is the most common and contagious form because it spreads through the air when an infected person coughs or sneezes (Photos: Envanto, Unsplash)
Pulmonary TB is the most common and contagious form because it spreads through the air when an infected person coughs or sneezes (Photos: Envanto, Unsplash)One night, I partied at the top of my lungs; the next day, I could barely move. I had a high-grade fever, sore throat, and a relentless cough. I popped a paracetamol, drank bitter kadhas, and tried to get on with my day—until the cycle repeated. I didn’t know a life-changing phase was awaiting me.
Even though I followed every instruction from my doctor—enduring distasteful medicines, nebulising thrice a day, missing work, surviving on daliya, khichdi and fruits—I kept burning up like a candle. My temperature stayed normal only during the fleeting four-hour window when medicines numbed my senses. I remember calling my mother at 3 AM once, unable to even pick up the medicine lying beside me. This went on for an entire month.
My bloodwork showed nothing dramatic, and the X-ray showed a mild lung infection. Of course, Google had its own terrifying theories—because what’s the internet for if not to raise your blood pressure with unsolicited medical advice? When the fever continued for weeks, my doctor grew concerned and referred me to a government hospital.
‘Nobody tested you for TB yet?’ one doctor asked. I went pale. Why would I even consider tuberculosis (TB)—a Victorian-era disease we rarely speak about? Isn’t this the same illness that wiped out entire populations? Soon enough, the dreaded words—Koch’s bacillus and pulmonary tuberculosis—appeared on my reports.
Turns out, I wasn’t alone in my shock. “Whenever I tell patients that the infection could be TB, their first reaction is denial—until I show them the reports,” says Dr Sagar Srivastava, Respiratory Medicine, Kailash Hospital, Greater Noida. Pulmonary tuberculosis is a bacterial infection that damages lung tissue, leading to cough, fever, weight loss, and weakened immunity. Left untreated, it can be fatal.
How you may miss the signs right in front of your eyes
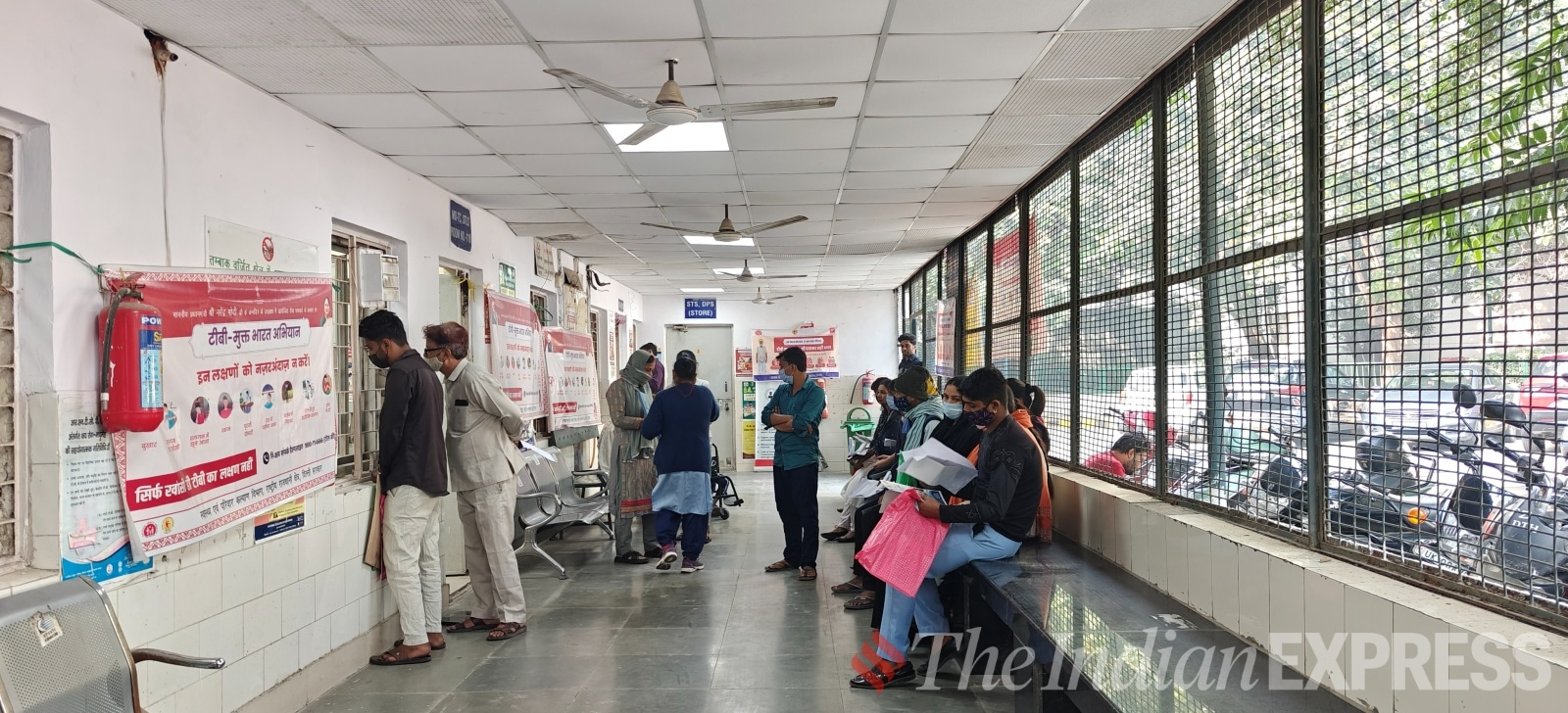 Patients waiting in the TB ward of Hedgewar Arogya Sansthan Hospital to collect their medication and gt pulmonologist’s consultation (Photo Credit: Vaibhavi Mishra)
Patients waiting in the TB ward of Hedgewar Arogya Sansthan Hospital to collect their medication and gt pulmonologist’s consultation (Photo Credit: Vaibhavi Mishra)
“I was lying in bed when I suddenly felt nauseated and coughed up blood for the first time. I thought I was dying,” recalls Sandeep Singh, a Delhi-based businessman.
After initial antibiotics, his symptoms eased, and blood tests looked normal. But when sharp chest pain set in, panic followed. “My family doctor immediately referred me to AIIMS. It took five to six days to get an appointment, but I was lucky the infection was caught in time,” he says.
Sunita Goyal, waiting at Delhi’s Dr. Hedgewar Arogya Sansthan to collect TB medicines for her 62-year-old husband, recounts a similar ordeal: “He had lung pain but normal blood tests, X-rays, and even three negative sputum tests. When breathing issues and fatigue increased, we went to Patel Chest Institute.”
Like them, my sputum tests were also repeatedly negative, even as my symptoms worsened. It was only when a chest CT scan was done that the real picture emerged.
This happens for several reasons—low bacterial count in early stages, poor sample quality, or the bacteria being outside the lungs in cases of extra-pulmonary tuberculosis. “Tuberculosis is often mistaken for pneumonia in its early stages because both affect the lungs, but pneumonia does not turn into TB — it can simply weaken immunity and unmask a hidden infection,” explains Dr Kashmira Jhala, Consultant Pulmonologist and International Sleep Disorder Specialist, Apollo Hospitals, Ahmedabad.
How does your body change during pulmonary tuberculosis?
 “Stigma around TB often comes from old beliefs that TB only affects poor or careless people, which is not true. Anyone can get TB,” clarifies Dr. Sunil Kumar K (Photo Credit: Express Photo Archive)
“Stigma around TB often comes from old beliefs that TB only affects poor or careless people, which is not true. Anyone can get TB,” clarifies Dr. Sunil Kumar K (Photo Credit: Express Photo Archive)
Dr Sagar explains that the intensity of infection and the body’s response to treatment vary from person to person. For some, the contagious period is brief; for others, it severely affects daily life.
Weight loss is one of the most visible symptoms—I am living proof. I lost several inches and was on a bland, minimal diet. Ironically, those unaware of my illness praised my ‘fitness transformation’. As I struggled to keep my body functioning, society’s beauty standards applauded me.
“My right lung was completely affected,” says Arachika Kapoor, a Delhi-based media professional. “Doctors suggested surgery to drain the liquid, but I opted for medication. The medicines made me nauseous, gave me rashes, and even caused facial swelling initially.”
“Treatment for TB usually involves taking a combination of antibiotics for six to nine months,” explains Dr Sunil Kumar K, lead consultant – interventional pulmonology, Aster CMI Hospital, Bengaluru. “Patients must follow the full course to prevent drug resistance.”
The medicines are indeed harsh. I often felt nauseated after my morning dose. “The medicines are so strong that even urine turns brown or reddish,” Singh adds.
Not everyone’s experience is equally severe. “Just some coughing and weakness, which happens with any illness,” says Roopvati, 70, currently under treatment at Karkardooma’s Delhi Government Dispensary. She beams in pride while telling that she did not even get a fever in the past 60 years but a recent brain surgery made her immunity low, leading to this infection.
Similarly, Singh also had a relatively controlled experience with his tuberculosis symptoms. “I am Type 1 diabetic and so my sugar consumption was already low. My diet, metabolism, and immunity were also good. TB infection could not spread so much in my case.”
How bad can it get?
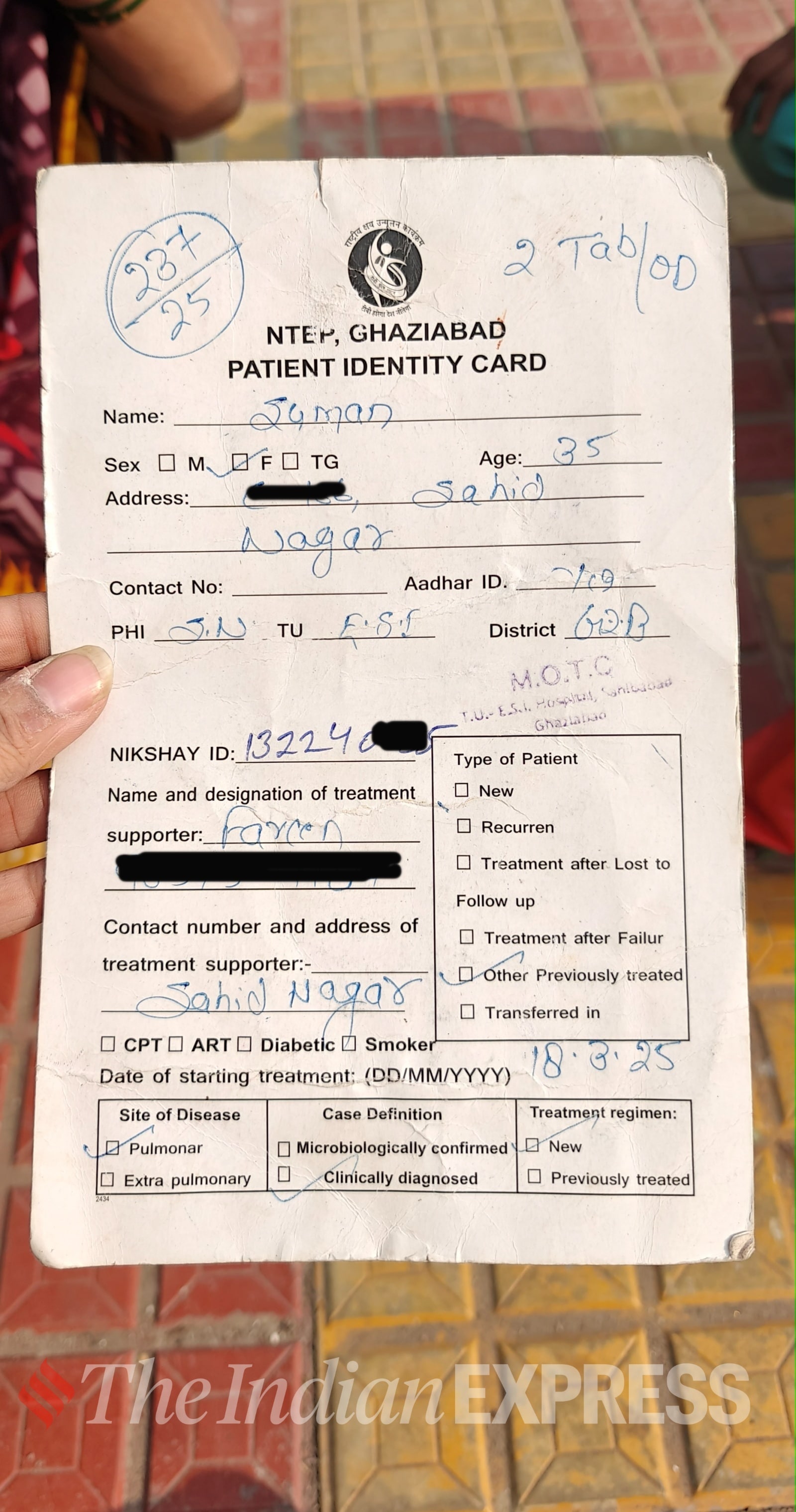 Every patient’s TB card has their Nikshay ID, treatment progress, test results chart, appointment dates etc. (Photo Credit: Vaibhavi Mishra)
Every patient’s TB card has their Nikshay ID, treatment progress, test results chart, appointment dates etc. (Photo Credit: Vaibhavi Mishra)
For Suman, 35, a patient slumped on Hedgewar Hospital’s floor, the pain is unbearable. “My chest hurts terribly; I feel like I’ll die coughing,” she says. Her husband, Raju, adds, “She was never like this. This disease has consumed her.”
Suman, a mother of one, is suffering from TB for the second time. Financial struggles make regular hospital visits difficult, and the couple fears this could affect their son’s education.
Dr Kumar warns that incomplete medication can lead to drug-resistant TB, which is harder to treat. “A healthy diet, rest, and avoiding alcohol and smoking are crucial for recovery,” he adds.
You’re not just a patient—you have a social responsibility
TB is highly contagious and spreads through coughing, sneezing, or even talking. “A patient can remain contagious for up to two months and must be isolated,” says Dr Sagar. Some people may also carry latent tuberculosis—infected but not diseased—yet capable of passing it to others.
Despite this, many patients ignore precautions. “People cough without covering their mouths or spit in public. These bacteria can survive on surfaces, infecting others,” warns Dr H C Sharma, medical superintendent, Kailash Hospital.
Dr Kumar adds that once medication begins, the bacteria count drops rapidly, and the risk of spread reduces. Still, patients should not return to work or public places without medical clearance. Masks are non-negotiable, and personal items like utensils, combs and clothes should be kept separate.
Why you now have a ‘Nikshay ID’
Given India’s high TB burden, the government closely monitors every case through the National TB Elimination Programme (NTEP), which aims to eradicate the disease by 2025 through free treatment, digital tracking, and community support.
Once diagnosed, patients are enrolled in the Nikshay system and assigned a unique ID to track their progress. I remember authorities calling patients who hadn’t turned up for doses, urging them not to discontinue treatment. The ID remains valid even if you switch hospitals.
When the government becomes your caretaker
 In many DOT centres, patients are not allowed to leave until they take the medicine infront of the authorities (Photo credit: Vaibhavi Mishra)
In many DOT centres, patients are not allowed to leave until they take the medicine infront of the authorities (Photo credit: Vaibhavi Mishra)
“You cannot leave the centre until you take your dose in front of the staff,” recalls Singh, who was treated at the AIIMS DOT Centre. I had a similar experience. In the early phase, patients must visit frequently so doctors can monitor their response before longer prescriptions are allowed.
Under the Nikshay Poshan Yojana, each patient is entitled to a monthly monetary allowance of ₹500–1,000 and sometimes, even a nutrition kit with peanuts, rice, oil, and pulses. The government paying and feeding me during my illness was something I never expected. Though my payment was delayed due to a bank issue, officials assured me it would be resolved. For families like Suman’s, such delays can be devastating.
Life after tuberculosis
Honestly, I sometimes forget I even had TB. There are no visible after-effects, though I tired easily for months. My appetite grew immensely, and I gained weight post-treatment. Dr Sagar notes that some patients are prescribed appetite stimulants, but the change varies.
Singh shares, “Everything is normal now, though my chest X-ray still shows a permanent patch on my lungs. Doctors confirmed it’s harmless.” Kapoor, however, still feels breathless. “I used to walk and run easily, but now I get tired quickly. I also catch colds far more often,” she says.
For some, tuberculosis leaves physical scars. For others, it’s the memory of the fight—and the surprising realisation that recovery brings not just health, but perspective.
DISCLAIMER: This article is based on information from the public domain and/or the experts we spoke to. Always consult your health practitioner before starting any routine.
📣 For more lifestyle news, click here to join our WhatsApp Channel and also follow us on Instagram


- 01
- 02
- 03
- 04
- 05

























