The Centre last week reviewed the rise in cases of influenza, and states have been readying hospitals for a possible spike in infections. The Union Health Ministry has confirmed a death each in Haryana and Karnataka due to the H3N2 subtype of the flu virus this month. Data from the Integrated Disease Surveillance Programme suggest at least nine people died of the flu in January.
There were 3,038 laboratory confirmed cases of the flu in the country until March 9 this year, show the latest data from the Ministry. This isn’t unusually high; 13,202 cases were reported in all of last year. To be sure, the number is likely an undercount because not everyone tests for the flu and not all test results are reported to the government.

Officials and experts said the current spike is because, first, this is the flu season. India usually sees two flu peaks every year — between January and March and, post-monsoon, between August and October. The virus spreads as the season changes. Besides the flu, a spike has been reported in the cases of other respiratory infections such as adenovirus and Covid-19.
Second, fewer flu infections during the pandemic has resulted in a large reservoir of people with lower immunity.
“Every year there is a subclinical spread of influenza and people acquire some immunity to it. But during the pandemic, people masked up, stayed away from crowded areas, avoided gatherings, and this spread could not occur. Hence, there is an increase this year,” Dr Sujeet Singh, Advisor and former director at the National Centre for Disease Control (NCDC), said.
The two pandemic years, 2020 and 2021, reported only 2,752 and 778 cases of the flu respectively.
Third, the flu virus is prone to changing its structure. “This means that we see an increase in flu cases usually every other year,” Dr Singh said.
Story continues below this ad
Fourth, India’s burden of conditions like diabetes and heart disease — which are risk factors for severe disease — is huge even among the young. The yearly flu shot is not readily available in government set-ups, and its uptake is not high.
At least two states, Gujarat and Maharashtra, have reported a new sub-variant of the novel coronavirus, XBB.1.16. However, very few genome sequences are available, and not much is known about the sub-variant yet.
Researchers have said that although there seems to be a growth advantage — seeing as it is replacing previously dominant variants — whether it could lead to a surge or to severe cases is not known. Hospitals are still reporting Covid-19 cases with upper respiratory tract symptoms and fever, similar to what is seen with the flu.
 Source: National Centre for Disease Control, ICMR Influenza database
Source: National Centre for Disease Control, ICMR Influenza database
So have Covid-19 cases spiked as well?
Larger numbers of Covid-19 cases have been reported over the last two weeks. But the base is low — weekly new cases increased from 2,082 during the week ended March 8 to 3,264 during the week ended March 15, according to government data.
Story continues below this ad
“Only 10% of patients hospitalised with respiratory symptoms in Delhi were found to have the H3N2 flu. Another 15% actually had Covid-19,” a senior health official said. New Covid infections had increased in the southern states and Gujarat over the last couple of weeks, the official said.
The Centre has written to six states — Tamil Nadu, Telangana, Kerala, Karnataka, Gujarat, and Maharashtra — asking them to carry out adequate and proactive testing, monitor new and emerging clusters of infections, keep an eye on influenza like illnesses (ILI) coming to health facilities, and send samples of international travellers, sentinel sites, and clusters for genomic sequencing.
Is it unusual for people to die of the flu?
It actually isn’t. While it causes mild symptoms like fever, cough, and runny nose in most people, like Covid, it can lead to complications like pneumonia and acute respiratory distress syndrome (ARDS) that can lead to death.
Very young children, old people, people with comorbidities such as heart disease, diabetes, and kidney disease, pregnant women, and those with a weakened immune system — such as people who have undergone transplants — are at higher risk of getting severe disease.
Story continues below this ad
Last year, there were 410 deaths due to the infection. While most were caused by the more common subtype H1N1 during the surge in respiratory infections in August, the ICMR’s network of viral diagnostic labs started detecting increasing numbers of H3N2 cases by December.
Is H3N2 a new sub-type of influenza?
No, it is one of the sub-types of the influenza virus that has been known to cause seasonal infections — just like the 2009 pandemic subtype H1N1 that has been in circulation since. In fact, H3N2 caused a flu pandemic back in 1968.
“The sub-type was detected in India in 1996 and has since caused outbreaks too. The only difference this year is that the disease seems to be a little more severe than we would usually see with H3N2,” a senior government official said.
It was the second most commonly found virus in respiratory samples during August-September 2021 surge — the most common being the Victoria sub-type. There are two main sub-types of influenza viruses: Type A has sub-types such as H1N1 and H3N2; the two lineages of influenza B are Victoria and Yamagata. Influenza A is usually associated with more severe disease and deaths.
Story continues below this ad
Why is the flu shot updated every year?
The list of subtypes to be included in the yearly flu shot is updated by the World Health Organisation twice a year depending on the types in circulation.
The ICMR network of viral laboratories test respiratory samples throughout the year from sentinel sites to keep an eye on the ups and downs in the numbers of flu cases, but more importantly to track the sub-types in circulation. There is a need to continuously update the vaccine because of the constantly evolving nature of influenza viruses.
It can undergo an “antigenic drift” to acquire mutations that change the part that cause the body to elicit an immune response. The Covid-19 equivalent would be the spike protein — which too has changed, though not enough to render a vaccine using the original virus useless.
It can also undergo an “antigenic shift” — an abrupt, major change that leads to a new protein structure of the virus. This results in a new virus from the same family infecting humans, or a virus that infects animals to jump over to humans. These shifts can lead to pandemics such as the one in 2009, or even the Spanish flu of 1918.
Story continues below this ad
The flu vaccine usually contains four subtypes — two each of influenza A (H1N1 and H3N2 are recommended for 2022-23) and influenza B.
What should be done to prevent infections?
Influenza spreads when people inhale infected droplets released by patients when they cough or sneeze. These droplets can survive on surfaces, and can spread if a person touches the surface and then touches their eyes, nose, or mouth.
Chances of transmission can be reduced by ensuring that the mouth and nose are covered when you sneeze or cough, and by washing hands frequently. It is best to remain at home when sick, and to drink plenty of fluids.
Story continues below this ad
Masks may be used in crowded places to prevent the spread of infection.



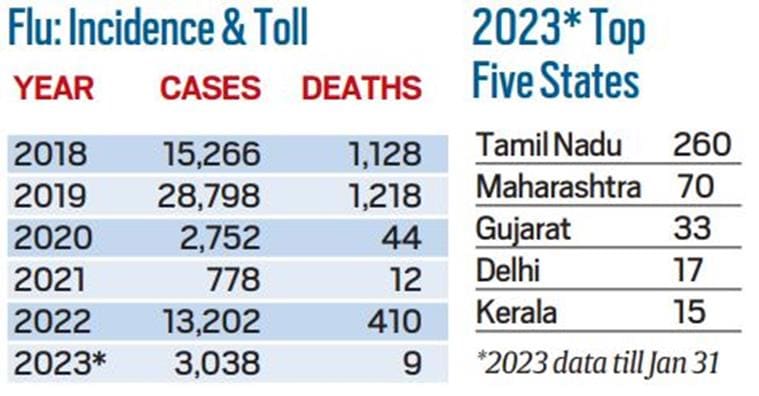 Source: National Centre for Disease Control, ICMR Influenza database
Source: National Centre for Disease Control, ICMR Influenza database