A set of new draft guidelines for UK’s National Health Service (NHS) calls for wider use of cholesterol-lowering drugs or statins, recommending that they be prescribed to even those who have less than 10 per cent risk of getting a heart attack or stroke over the next ten years. With the risk of cardiovascular events being higher among South Asians, Dr V Mohan says that the medicine should be more readily prescribed in India. The uptake of the life-saving drug unfortunately, he says, continues to be “abysmally low” in the country.

To answer that, we need to first look at how this 10 per cent risk is calculated. There are several risk scores that have been developed over the years; none of them is suitable for South Asians. The assessment is based on data from the Western population that has a lower risk of heart diseases. South Asians are much more prone to atherosclerosis (narrowing of the blood vessels due to cholesterol deposition) and Type-2 diabetes, and early on, even with thinner structures.
Story continues below this ad
We can follow this assessment but it under-predicts the risk for us. What this essentially means is that if someone comes in with high levels of cholesterol, we have to treat that condition. The initiation of treatment does not depend on this 10-year risk of cardiovascular diseases.
Besides, statins are used to bring down the levels of low density lipoprotein (LDL) or bad cholesterol. This is because LDL cholesterol is produced inside the body, within the liver. Statins have also been shown to have anti-inflammatory effects (which may slow the progression of disease). Additionally, high levels of triglycerides have to be treated, otherwise they can lead to pancreatitis (inflammation of the pancreas). There are different medicines for triglycerides because diet and exercise are not very effective in lowering them.
Do we have a similar model in India to predict risk?
Not at the moment but work is ongoing. The thing is to develop such a score, long term data from a large cohort is needed on the baseline and the number of deaths over ten years. This cannot be done with data on, say, 50 deaths. We would need to observe somewhere around 2,000 deaths due to cardiovascular events to calculate the risk factor and predict accurately.
Story continues below this ad
The process of generating this data has already started and we may have scores based on the Indian population in the next two to three years. Having a model based on Indian data would not only help clinicians identify who should get the treatment and when but also what the targets and doses of medicines should be.
Does the higher risk in the Indian population mean anyone with high levels of cholesterol should be started on statins?
No. The overall picture has to be taken into account. If a 20-year-old comes with slightly elevated LDL levels, we might try lifestyle interventions like diet and exercise, with the medicine being prescribed only if the levels still continue to be high. This is because statins have to be taken for life. But if the same person with the same LDL levels has parents who have had a heart attack at a young age, then treatment must be initiated.
The treatment also has to be more aggressive in those who have diabetes, as that is independently a risk factor for cardiovascular diseases. In fact, the history of diabetes is considered equivalent to a history of heart attack. Currently, statins are prescribed only to those people who have LDL levels of 130 with diabetes or more than 160 without diabetes. They should be prescribed to those with family history of heart disease, those who have had a heart attack or have undergone stenting.
Story continues below this ad
Statins are harmless drugs – except for some muscle pains reported in few – and have been shown to reduce cardiovascular events in several studies.
Are statins widely in use in India?
Unfortunately, no. India’s average is abysmally low, even among those who have had a heart attack. Statins should be taken by 100 per cent of those who have had a heart attack but not even one-third take it. This is because of costs as the medicine needs to be continued for life.
But hesitancy is also because of a lot of misinformation on social media saying that statins are a conspiracy of big pharma and that there is nothing called cholesterol. People also ask when they can stop taking the medicine, worried about “side effects.”
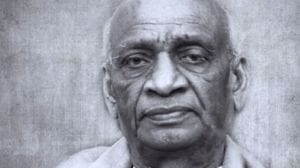
Why Dr V Mohan? Dr Mohan is a renowned diabetologist and the chairman of Dr Mohan’s Diabetes Specialities Centre. He is also the president of the Madras Diabetes Research Foundation, which is an ICMR-advanced centre for studying the genomics of Type-2 diabetes. He has over 1,500 publications. He has also received the highest honour for doctors in India Dr BC Roy Award and the fourth-highest civilian award Padma Shri.