In 16 districts, fatality rate due to black fungus higher than state average
As of November 2021, a total of 9,961 Covid-19 patients contracted mucormycosis. Of these, 1,300 succumbed to the infection. Most of these cases came from rural districts where the healthcare accessibility was constrained.
 A doctor from Raigad said that as per treatment protocol, when the black fungus infects the nose, sinus or palate, doctors are supposed to administer 5mg of dose for each kilogram (kg) of body weight.
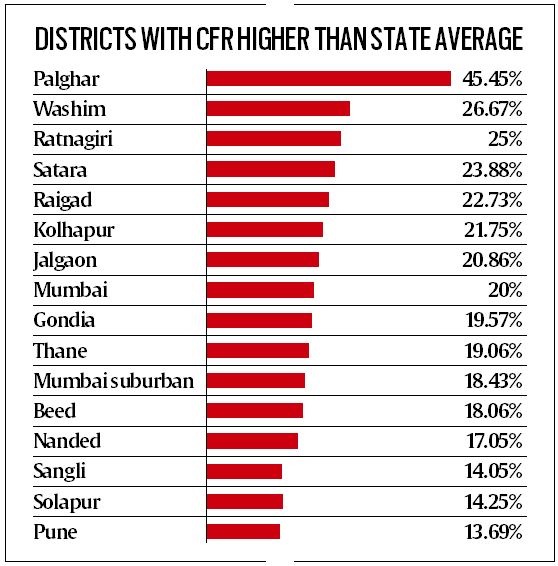
A doctor from Raigad said that as per treatment protocol, when the black fungus infects the nose, sinus or palate, doctors are supposed to administer 5mg of dose for each kilogram (kg) of body weight. Sixteen districts in Maharashtra had a case fatality rate (CFR) of Covid-associated mucormycosis or black fungus substantially higher that the state average of 13.4 per cent recorded during the second wave of the pandemic in 2021, according to government data. Experts said the high CFR recorded in these districts was largely due to the “broken down” health care system as well as unavailability of life-saving, expensive medicines and absence of specialist doctors.
A few districts, including Mumbai, had a CFR greater than 20 per cent. These include Palghar (45.45 per cent), Washim (26.67 per cent), Ratnagiri (25 per cent), Satara (23.88 per cent), Raigad (22.73 per cent), Kolhapur (21.75 per cent) and Jalgaon (20.86 per cent). Experts attributed Mumbai’s CFR – 20 per cent – to the volume of patients being referred from other districts.
As of November 2021, a total of 9,961 Covid-19 patients contracted mucormycosis. Of these, 1,300 succumbed to the infection. Most of these cases came from rural districts where the healthcare accessibility was constrained.
One such victim was 52-year-old Amrita Salvi, who caught the fungal infection after being discharged from the Beed civil hospital after being treated for novel coronavirus. “Soon, we noticed the blackening of the skin inside her mouth,” said Ramesh, her son.
Salvi was admitted to a private hospital in Beed, but by then the infection had crept up her nose. She underwent two surgeries. The doctors prescribed 100 vials of liposomal amphotericin B injection. But by then, the number of patients suffering from mucormycosis had surged to 5,644 in the state, leading to a shortage of the drug.
On May 22, Salvi succumbed to the infection and the family had to pay Rs 5 lakh to the hospital for her treatment.
Dr Mangala Gomare, executive health officer, Brihanmumbai Municipal Corporation, said, “Nearly 80 per cent of the cases that we recorded in Mumbai were patients referred from other cities. Due to lack of health facilities and ENT specialists, patients from far-off districts also approached us.”
Mucormycosis is a rare infection caused by a group of moulds called mucormycetes. Doctors from rural districts blamed the government for ignoring their parts of the state when Maharashtra was facing shortage of Liposomal Amphotericin B and plain Amphotericin B.
A doctor from Raigad said that as per treatment protocol, when the black fungus infects the nose, sinus or palate, doctors are supposed to administer 5mg of dose for each kilogram (kg) of body weight. But when the infection reaches the brain, doctors have to give 8-10mg of the drug for each kg of the body weight. “But as
the district didn’t have the supply, we had to use the available vials reasonably on patients. Their
kin would travel to other districts to procure the medicines,” said a doctor, who was involved in treatment of Covid-19 patients in the district hospital. An official, earlier associated with the health department, said that in the second wave, the demand suddenly increased from seven persons contracting the black fungus in December 2020 to over 600 in April 2021. “The Centre had provided just 18,000 injections in May… Later, the state had to procure directly from the manufacturers at a higher rate,” said the officer.
Bombay Hospital’s Dr Gautam Bhansali, who was in-charge of Covid beds in private hospitals, said that as doctors stationed in primary health centres and rural hospitals weren’t qualified to identify mucormycosis, they would ignore it as a mere rash. “Rural centres often lack CT or MRI facilities or specialists to collect samples for fungal culture,” he added.