In Nandurbar, with no proper treatment, sickle cell anaemia patients develop deformities, even die
Without proper treatment, patients develop deformities and some even succumb, of which there are no records.
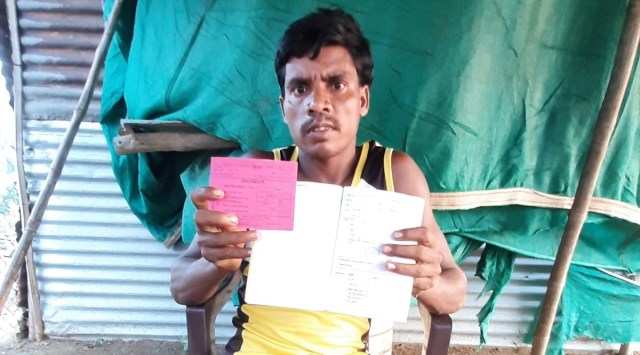 Burshalal Vasane shows his sickle cell card. (Express Photo)
Burshalal Vasane shows his sickle cell card. (Express Photo) Nandurbar district, which has a predominantly tribal population, has the most number of sickle cell anaemia (SCA) patients in the state. Despite having the highest number of cases of the life-threatening blood disorder, the district lacks basic health infrastructure, medicines and specialists to treat the disease.
Without proper treatment, patients develop deformities and some even succumb, of which there are no records.
Burshalal Vasane’s right leg is slightly bent inward and he walks with a stick. “The blood flow in my right leg has been obstructed, leading to the deformity,” said Vasane (37), a resident of Danel village. For Vasane, living with the disease for over three decades hasn’t been easy. On days when he reels in pain, he is referred from one primary health centre (PHC) to another.
Sickle cell anaemia is a genetic or hereditary disorder, in which red blood cells become oval-shaped due to oxygen deficiency in blood. It occurs when a person inherits two abnormal copies of the haemoglobin gene from each parent.
According to government data, Nandurbar has over 21 per cent of the state’s sickle cell anaemia patients. Of the 18,000 registered patients, 3,842 are from Nandurbar. A study — ‘Sickle Cell Anaemia in rural areas of Nandurbar district’, conducted between 2009 and 2015, showed that Dhadgaon and Nandurbar talukas topped the list, comprising 0.36 per cent and 0.27 per cent of the cases, and 3.65 per cent and 1.30 per cent of the carriers, respectively. Mortality was highest below the age of 10 years.
Common among infants and children, the disease causes severe body ache, infections, fatigue, weakness, hemoglobinopathies (destruction of blood cells), bone necrosis and even strokes. Treatment comprises lifetime medication, where the patient is given folic acid and Hydroxyurea, a medicine that makes the red blood cells bigger.
Doctors and patients, however, complained that often there is a dearth of Hydroxyurea in the district. Patients are often sent back with painkillers and folic acid. This forces the tribals to rely on alternative healers for pain relief. “As SCA is considered a disease of the poor unlike thalassaemia, the investment and initiatives are less. It is considered a neglected disease,” said Dr Jibi John, internal medicine specialist at Chinchpada Christian Hospital at Chinchpada in Navapur taluka.
Sometimes, villagers sell their agricultural land or spend all their savings to treat their children in private hospitals. For instance, Kalu Singh Valvi, a resident of Katri village in Akarani taluka, has to travel for three hours to reach Chinchpada Christian Hospital — run by doctor couple Dr Deepak Singh and Dr Ashita Singh — for his seven-year-old son’s treatment.
“As no public transport is available, I have to take a shared cab which costs Rs 4,000. His monthly medication costs another Rs 400,” said Valvi, a farmer.
Mohan Vasave was only six months old when he was diagnosed with SCA. In 2019, he was rushed to the PHC at Roshmal village in Akarani. “They just gave him a pain injection. He was sent home but soon the pain restarted. He had to be admitted in a private hospital,” said Saisingh Vasave, his uncle. It cost around Rs 25,000. In September, he again had to be admitted in an ICU in a private hospital for blood transfusion.
Speaking about paediatric patients, Dr John said that per kg of weight, 5 mg of Hydroxyurea dosage is allowed. “Now, if a child is 10 kg, we recommend 50 mg dosage. But as the liquid isn’t available, we have to open the capsule, blindly gauge the dosage to be given to the child. This is so unscientific as one isn’t supposed to open the capsules, which can reduce its efficiency.”
The disease can be cured with bone marrow transplant but a RTI filed with the district health authorities had revealed that Nandurbar doesn’t have a single bone marrow centre.
“Severely ill patients where bone marrow transplant is the only hope of survival are being sent to Nashik or Mumbai government hospitals. In private hospitals, it costs over Rs 25 lakh,” said Gautam Dongre, secretary of National Sickle Cell (NASCO). Some patients often need immediate blood transfusion but finding a blood bank is another uphill task.
The state, meanwhile, lacks data of the total number of fatalities related to sickle cell anemia. Dr Mahendra Kendre of the state’s Directorate of Health Service, said that there is no mechanism to check if a patient has died.
Dr Govind Choudhary, district health officer, said they regularly hold health camps where they test tribal children for sickle cell anaemia. “Our Asha workers regularly follow up with the families to check if they are taking the medicines. The district civil hospital also has a unit for the treatment of patients with sickle cell anemia,” he said.
Under Sanjay Gandhi Niradhar Anudan Yojana, patients with SCA who have suffered any kind of disability and whose family annual income is up to Rs 21,000 are liable to get Rs 600 allowance per month. But due to lack of awareness and bureaucratic apathy, many like Vasane haven’t received the benefits. “SCA has been added in the list of differently-abled welfare schemes but most patients are unaware of it,” said Dongre.