Stay updated with the latest - Click here to follow us on Instagram
HPV vaccine delay risks lives: Nearly 4,000 women die from cervical cancer in Maharashtra in six years
Cervical cancer occurs in the cervix, the lower part of the uterus that connects to the vagina, and is most commonly caused by human papillomavirus (HPV).
In February, Finance Minister Nirmala Sitharaman announced the Centre’s plan to include HPV vaccine that protects against cervical cancer in the national immunization programme. However, nine months later, the state health department is yet to receive an official directive from the Centre, with doctors warning that this delay could put many lives at risk, especially given the high mortality rate from preventable cervical cancer.
According to data from The Indian Express, between 2017 and 2022, a total of 3,941 women in Maharashtra died from cervical cancer, with over 657 deaths per year on average. Health experts have stressed the urgent need for the HPV vaccination, which could potentially reduce the burden of cervical cancer-related fatalities.
monthly limit of free stories.
with an Express account.
“We haven’t received any instructions from the central government regarding HPV inclusion in the national immunization programme. Even if they approve, we will need additional funds for manpower,” said a senior officer from the state health department.
“The department has received two requests from municipalities in the state to start the immunization, and we are in the process of issuing the no-objection certificate,” the officer added. District medical officers frequently inquire about initiating the HPV vaccination programme, indicating a rising demand for the vaccine at the local level.
Cervical cancer occurs in the cervix, the lower part of the uterus that connects to the vagina, and is most commonly caused by human papillomavirus (HPV). While many HPV infections clear on their own, strains such as HPV16 and HPV18 are linked to cervical cancer. HPV is most commonly transmitted through sexual activity, particularly in individuals with multiple sexual partners. The infection can lead to cancer if not detected early.
Data from the state health department reveals fluctuations in cervical cancer-related deaths over the past few years. In 2017, 546 women died from cervical cancer, but this number rose sharply to 1,073 in 2018.
The death toll dropped to 673 in 2019 but then plummeted to 532 in 2020, likely due to the restrictions imposed during the Covid-19 pandemic, which hindered access to healthcare and cancer detection services. In 2021, the number of deaths increased again to 722. However, in 2022, the death toll decreased to 395.
As of 2022, more than 125 countries have included the HPV vaccine in their national vaccination programmes, recognizing its potential to prevent cervical cancer. The World Health Organization (WHO) lists the HPV vaccine as an essential medicine, stating that expanding access to vaccines is a crucial step in reducing cervical cancer-related deaths worldwide.
“The most important step to prevent cervical cancer is to get vaccinated against HPV at a young age, ideally before sexual activity begins,” said Dr. Sewanti Limaye, director of oncology and precision medicine at HN Reliance Hospital.
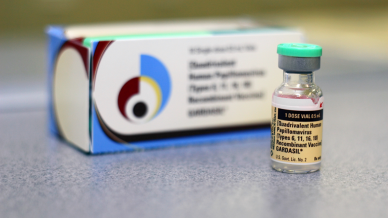
Currently, two HPV vaccines are available in India—Gardasil (quadrivalent) and Cervarix (bivalent)—with costs of Rs 2,800 and Rs 3,299 per dose, respectively. The high cost of these vaccines is a significant barrier, especially for women in rural areas or those with limited financial resources, preventing them from seeking vaccination at private healthcare centers.
Dr. Nikhil Datar, senior gyneacologist and medical director at Cloudnine Group of Hospitals, outlined that cervical cancer incidence is notably high in India, and early detection remains a significant challenge. The disease often progresses without noticeable symptoms, making it difficult to identify in its early stages.
“By the time symptoms appear, cancer is typically advanced, limiting treatment options and outcomes. Vaccination with HPV vaccines like Gardasil and Cervarix has shown clinical effectiveness in preventing infection from high-risk HPV strains responsible for the majority of cervical cancer cases. If included in the national immunization program and provided free of cost, this vaccine could drastically reduce cervical cancer incidence and related fatalities in India,” he added.